The table of content
Introduction: Medicine is Changing — and Fast
Cardiovascular disease (CVD) remains the leading cause of death worldwide, claiming over 17 million lives every year. Despite breakthroughs in medicine, too many people still lose their lives to heart problems that could have been prevented. The challenge isn’t what we know—it’s how we apply it.
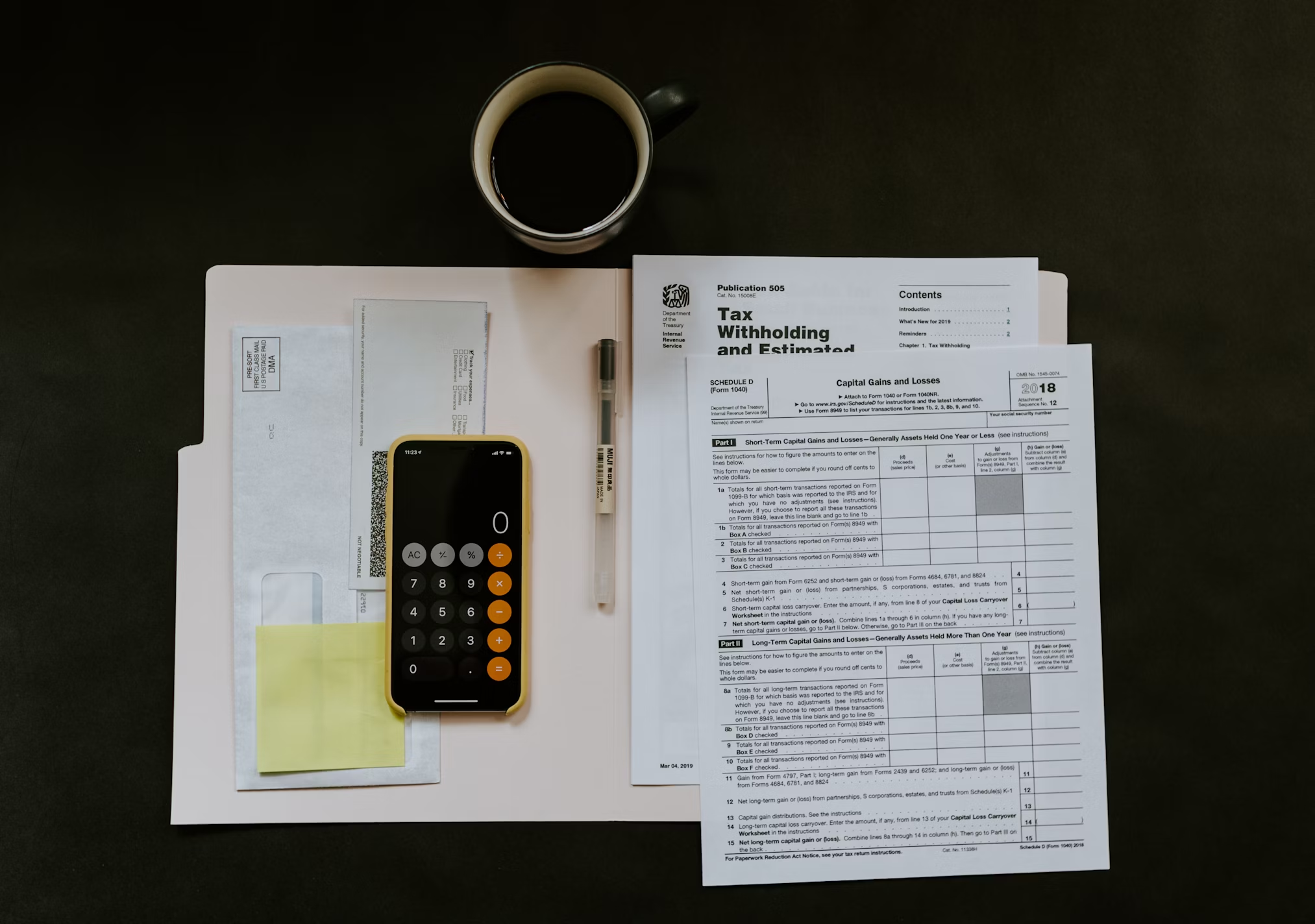
Traditional heart diagnostics rely on expensive, invasive tests and repeated doctor visits. Healthcare systems simply cannot afford to screen entire populations this way. That leaves countless high-risk individuals invisible to the system—until it’s too late.
But what if we turned the system on its head? Instead of waiting for symptoms to appear, what if we could predict risk early, using the data people already generate in their daily lives? This is where predictive analytics comes in.
Predictive analytics is a branch of data science that takes historical information, feeds it through machine learning algorithms, and produces forecasts about future outcomes. For cardiovascular disease, that means building models that can flag people at risk before a heart attack or stroke ever happens—without needles, hospital beds, or endless appointments.
One case study illustrates the promise of this approach. Researchers applied predictive modeling to health data from more than 20,000 individuals. The model detected cardiovascular risk factors with striking accuracy, allowing doctors to identify at-risk patients long before traditional methods would have.
The impact is twofold: medically, it opens the door to earlier interventions that save lives; commercially, it creates scalable, cost-effective tools that could ease the burden on overwhelmed healthcare systems.
In other words, the future of heart health might not lie in more stents and surgeries, but in smarter data. Predictive analytics could shift the fight against cardiovascular disease from treatment to prevention—catching silent risks before they roar into crisis.
The Challenge: Detecting Risk Without Touching the Patient
The toughest part of fighting cardiovascular disease isn’t the treatment—it’s finding out who is at risk before the damage begins. Traditional tools like electrocardiograms, stress tests, or CT scans can reveal a lot, but they come with heavy trade-offs. They’re expensive, take time to administer, and can only reach a fraction of the population. For healthcare systems already stretched thin, mass screening simply isn’t realistic.
That means doctors are often forced into a reactive role, stepping in only once symptoms surface or an emergency strikes. By then, options narrow and outcomes worsen. To change that pattern, researchers asked a different question: what if we could predict heart risks in advance, at scale, using the information people already generate in daily life?
The goal was to design a system that could process enormous streams of health and lifestyle data, then highlight individuals at elevated risk—without requiring them to set foot in a clinic. Building such a solution demanded more than medical know-how; it called for advanced data science. Machine learning models had to be trained to recognize subtle patterns across thousands of variables, from blood pressure history and lab results to demographic factors and lifestyle behaviors.
The result is a shift in mindset: away from episodic testing toward continuous, data-driven monitoring. With predictive analytics, healthcare providers don’t have to wait for the heart to show warning signs—they can intervene earlier, guiding patients toward prevention rather than crisis care.
The Solution: A Data-Driven Model with 94% Accuracy
To address the problem, researchers built a predictive model using data from more than 20,000 individuals. The dataset was enormous—not just in size but in dimensionality. It included over 350 variables per person, covering everything from demographic traits and economic indicators to environmental conditions and previous medical history.
After processing and training, the model selected 75 of the most influential factors that strongly correlated with cardiovascular outcomes. These variables weren’t just medical, but included behavioral and regional characteristics, offering a more holistic view of what drives cardiovascular risk. For instance, a person’s access to clean air, stable income, or even walkable streets could indirectly affect their likelihood of developing heart disease.
The model's performance was impressive. It achieved a Gini index above 94, indicating excellent discriminatory power between high-risk and low-risk individuals. Its AUC (Area Under the Curve) score, a standard benchmark for model quality, approached 0.97 on both the training and test datasets—evidence that the model was not only accurate but also generalizable.
Most notably, the model was able to identify 95% of high-risk individuals without any medical testing or direct patient interaction. In other words, it could predict risk as accurately as some diagnostic tests, but at a fraction of the cost, and without needing to draw blood or administer an EKG.
Real-World Impact: Better Care, Smarter Business
The implementation of this predictive system brought immediate benefits to healthcare providers. First and foremost, it allowed medical teams to prioritize patients more effectively. Instead of using generic age-based screenings or waiting for symptoms to appear, providers could now focus their resources on people who were statistically most likely to develop cardiovascular issues. This improved treatment outcomes while simultaneously reducing the cost burden on the system.
In addition to its clinical value, the model also opened up new business opportunities. Providers were able to offer predictive health services as part of wellness programs, positioning themselves as forward-thinking institutions focused on prevention rather than just treatment. These services attracted both individual patients and insurance companies looking for proactive ways to reduce long-term healthcare costs.
Moreover, the model enabled providers to personalize their outreach. Individuals flagged as high risk could be invited for targeted check-ups, consultations, or lifestyle intervention programs. Instead of sending the same generic health reminders to everyone, clinics could now communicate with patients in a way that felt timely, relevant, and meaningful. That kind of personalization not only increases engagement but also builds trust.
In a market where healthcare is becoming more competitive, predictive models like this offer a compelling advantage. They empower providers to move from reactive treatment to proactive prevention, and from one-size-fits-all medicine to data-driven personalization.
Why This Matters: A Paradigm Shift in Public Health
The implications of this model reach far beyond cardiovascular disease. At its core, it signals a paradigm shift in public health—moving from a system that reacts to illness toward one that anticipates and prevents it.
We’ve seen similar transformations in other industries. Streaming services suggest what to watch, online stores predict what you might buy next. In healthcare, the stakes are higher, but the logic is the same: instead of recommending a playlist, a predictive model can suggest a diagnostic test or a lifestyle change—actions that may literally save a life.
This kind of intelligence is especially valuable in overstretched healthcare systems, where universal screening is impossible. By concentrating resources where the risk is highest, predictive analytics allows providers to do more with less. The strategy is both efficient and deeply humane—acknowledging the limits of existing systems while using data to extend their reach.
Limitations and Ethical Considerations
Of course, no system is flawless—and predictive analytics is no exception. The power of these models rests entirely on the data they’re trained with. If that data skews toward certain groups—say, urban populations with regular access to hospitals—then people outside those groups risk being misrepresented. In some cases, existing inequalities can even be amplified by the very tools meant to reduce them.
Privacy adds another layer of complexity. Even when data is anonymized and encrypted, the idea of predicting someone’s future health condition without their knowledge raises valid ethical questions. Who owns the predictions? How should they be shared? Ensuring transparency, informed consent, and robust data protection isn’t optional—it’s the foundation on which trust in these systems will stand or collapse.
There’s also the human side of adoption. A predictive model is not a crystal ball—it’s a decision-support tool. Doctors and nurses must be trained to interpret risk scores, weigh them against clinical context, and communicate them clearly to patients. Used well, these tools extend human expertise; used poorly, they could overwhelm or mislead.
Predictive analytics, then, is not about replacing human judgment with algorithms. It’s about giving healthcare professionals sharper instruments, while remembering that the skill of the surgeon still matters more than the sharpness of the scalpel.
Conclusion: The Future is Already Here
This case study shows just how transformative predictive analytics can be in healthcare. Using only existing data—no blood draws, no scans, no hospital visits—a machine learning model was able to flag cardiovascular risk with 95% accuracy. That’s not a futuristic dream; it’s a present-day reality.
The implications are enormous. Patients benefit by getting care earlier, often before a crisis ever occurs. Providers can allocate their limited resources more effectively, focusing attention where it’s needed most. Entire populations can be screened at a fraction of today’s cost, breaking through barriers that have long made preventive care difficult to scale.
Most importantly, the very philosophy of healthcare begins to shift. Instead of reacting to illness once it becomes visible, systems can anticipate risk and intervene before the damage is done. It’s the difference between rushing to treat a heart attack and preventing one altogether.
As this technology spreads, the debate won’t be about if we should adopt predictive analytics—it will be about how fastand how responsibly we can make it a standard part of care. Because when it comes to saving lives, the ability to see trouble coming may be the most powerful medicine we’ve ever had.













.avif)

































.png)
.png)
